Regional difference in ventilation, Pulmonary circulation, Shunt and Lung perfusion zones
Global ventilation of the lungs is expressed as the minute volume, normally around 4L/min, This is affected by multiple factors, most notably pregnancy, PaCO2, PaO2, pH, body temperature, exercise, and blood pressure, Global perfusion of the lungs is directly proportional to the cardiac output (normally 5L/min), so, It is affected by all the factors which affect cardiac output, which include exercise, metabolic rate, volume-sensing reflexes, autonomic tone, etc.
Regional difference in ventilation
In the standing position, gravity pulls the lung down. This makes the IPP at the apex of the lung more negative than at the base, IPP at the apex -10 cm H₂O and at the base it is -2.5 cm H₂O at the mid-thoracic position. Therefore, the upper part of the lung at the end of normal expiration is more expanded than the lower part. More air is directed to the lower part during inspiration to the lower part of the lung is more ventilated than the upper part.
Pulmonary circulation
Pressures within and around the pulmonary blood vessels:
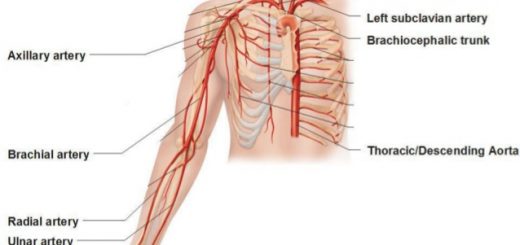
The pressures in the pulmonary circulation are remarkably low. The mean pressure in the main pulmonary artery is only about 15 mm Hg; the systolic and diastolic pressures are about 25 and 8 mm Hg, respectively. The pressure is therefore very pulsatile. By contrast, the mean pressure in the aorta is about 100 mm Hg-about 6 times more than in the pulmonary artery.
The pressures in the right and left atria are not very dissimilar-about 2 and 5 mm Hg respectively. Thus the pressure differences from inlet to outlet of the pulmonary circulation is about (15-5) = 10 mm Hg and systemic circulation is about (100-2) 98 mm Hg.
In keeping with these low pressures, the walls of the pulmonary artery and its branches are remarkably thin and contain relatively little smooth muscle (they are easily mistaken for veins). However, in the systemic circulation, the arteries have thick walls and the arterioles have abundant smooth muscles.
The reasons for these differences become clear when the functions of the two circulations are compared. The systemic circulation regulates the supply of blood to various organs and body parts, including those which may be far above the level of the heart (the upstretched arm, for example).
By contrast, the lung is required to accept the whole of the cardiac output at all times, and its arterial pressure is therefore as low as is consistent with lifting blood to the top of the lung. This keeps the work of the right heart as small as is feasible for efficient gas exchange to occur in the lung.
Capillary pressure
Pulmonary capillary pressure is about 10 mm Hg, whereas the oncotic pressure is 25 mm Hg, so that there is an inward-directed pressure gradient of about 15 mm Hg which keeps the alveoli free of fluid. When the pulmonary capillary pressure is more than 25 mm Hg in pathological conditions this will lead to pulmonary congestion and oedema.
Shunt
Shunt is the passage of deoxygenated blood from the venous circulation to the arterial side of the circulation without picking up O₂.
Physiological shunt
Refers to the normally present shunts that carry deoxygenated blood to the left side of the heart or to the pulmonary veins.
- The thebesian circulation perfuses the left ventricle myocardium and empties deoxygenated blood directly into the left ventricle.
- Some of the deoxygenated blood coming from the bronchial circulation empties into the pulmonary veins which also contributes deoxygenated blood to the arterial circulation.
These physiological shunts have normally a value less than 5% of the cardiac output and are responsible for making the O₂ saturation of the arterial blood 97% but never 100% even if 100% O₂ is inspired.
Distribution of pulmonary blood flow
Perfusion of lung tissue is dependent on the interrelationships between alveolar, arterial and venous pressures. The pulmonary circulation is normally a low-pressure circuit. Blood must be pumped as high as the apex of the lung, a distance of 15 to 20 cm above the heart which is a large distance for a low-pressure system as the pulmonary circulation.
Lung perfusion zones
Zone I
The pulmonary arterial pressure falls below alveolar pressure, thereby collapsing the alveolar vessels (capillaries are squeezed shut) and flow ceases. Pulmonary arterial pressure is normally just sufficient to maintain perfusion, but if is reduced (hemorrhage) or if alveolar pressure is increased (positive pressure ventilation), some of the capillaries collapse (zone of no flow). Under these circumstances, no gas exchange takes place in the affected alveoli and they become part of the physiologic dead space.
Zone II
As the vertical distance above the level of the heart decreases, local arterial pressure increases and finally exceeds alveolar pressure. Under these circumstances, blood flow is controlled by the difference between arterial and alveolar pressures. Venous pressure still has no effect on flow because it remains subatmospheric at this point in the lung.
Perfusion then increases dramatically in a linear fashion with decreasing vertical height because arterial pressure increases linearly with distance but alveolar pressure remains constant. Blood flow in zone Il is termed the vascular water-fall since flow is unaffected by downstream (pulmonary venous) pressure.
Zone III
In zone III venous pressure now exceeds alveolar pressure and flow is determined in the usual way by arterial-venous pressure difference. Zone III is characterized by a constant driving force i.e. both pulmonary artery and venous pressure increase in direct proportion to the decrease in the vertical distance but their difference remains constant.
Ventilation-perfusion relationships and why is ventilation higher at the base of the lung
Normal & abnormal lung compliance, Elastance, Surfactant and work of breathing
Mechanics of Pulmonary Ventilation and Pressure changes during Respiratory cycle
Diaphragm anatomy, structure, function, Phrenic nerves and Nerves of the thorax
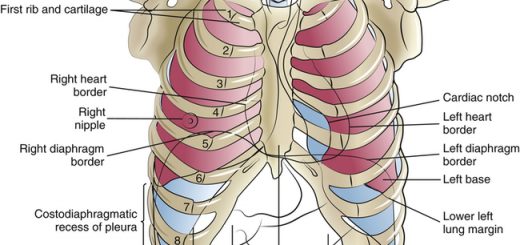
Lung structure, borders, Lobes, Fissures and Broncho-pulmonary segments
Larynx structure, function, cartilages, muscles, blood supply and vocal folds