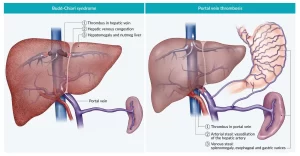
Diagnosis of Chronic or subacute Budd-Chiari syndrome and Risk Factors of Portal vein thrombosis
Chronic or subacute Budd-Chiari syndrome should be considered in unexplained liver dysfunction (in the laboratory test), particularly if ascites is a principal feature, or if risk factors for Budd-Chiari syndrome exist.
Clinical diagnosis of Budd-Chiari syndrome
- Splenomegaly, venous collaterals (Dilated veins on the abdomen and its direction is mainly from the downward upward and these are the collaterals that bypass the site of obstruction).
- Edema of the lower extremities suggests occlusion of the inferior vena cava (Which drains the lower limbs). But if there was obstruction of one of the 3 hepatic veins there won’t be L. L. edema unless there is an advanced cirrhosis with hypoalbuminemia.
- Signs of right-sided congestive heart failure (such as jugular venous distension.
- The incidence of Budd-Chiari syndrome is not high in chronic liver disease.
Laboratory/Radiology
1) Doppler ultrasonography
We will ask for the investigations which delegate the blood vessels. We use Doppler ultrasound as a Screening test, Doppler ultrasound is incorporated into the ultrasound apparatus. Ultrasound is an operative dependent which means that it depends on the skills of the operator in interpretation the findings. It is better than CT or MRI as it is small, cheap, easy, no radiation exposure and is available in most places. It is used to detect:
- if the blood vessel is patent or occluded partially or totally and measures the segment which is occluded and as the normal ultrasound, it can detect the size of the liver and spleen and if there are collaterals or any hepatic lesions.
- Hepatomegaly.
- Splenomegaly.
- Ascites.
- Intraabdominal collaterals.
- Caudate lobe hypertrophy.
- Atrophy of other hepatic lobes.
- Compression of IVC,
- Thickening, irregularity, stenosis, or dilation of the walls of the hepatic veins, Abnormal flow in the major hepatic veins or IVC.
2) CT scan
- It is used to confirm the findings of the ultrasound.
- If there aren’t findings in the ultrasound but we highly suspect Budd-Chiari syndrome, we do CT venography by using a contrast which enters the 3 hepatic veins and the IVC then captures a graph of the blood vessels or the venous drainage.
- It shows:
- Delayed or absent of the 3 major hepatic veins.
- Patchy flea-bitten appearance of the liver.
- Rapid clearance of dye from the caudate lobe.
- Narrowing and/or lack of opacification of the IVC.
3) Magnetic resonance imaging
We can replace the CT venography with an MRI venography .
It shows:
- Typical distorted “comma-shaped” intrahepatic Collaterals.
- Unremarkable ultrasound examination but in whom the suspicion is high.
4) Venography
- The normal venography, in which we inject contrast in the blood vessel with a catheter, became absolute and not needed because it has been replaced with CT and MRI venography which are less invasive and produce a better resolution and graphs.
- Plan therapeutic interventions.
- Determine the pressure gradient above and below the entrance of the hepatic veins into the inferior vena cava.
Treatment
- Identify and manage the predisposing factor and the original disease.
- Prevent the propagation of the clot and prevent its extension to another segment or another blood vessel.
- Decompress the congested liver As the liver is congested due to the occlusion of the venous drainage and
- ischemia happens because the blood supply isn’t efficient.
- Prevent complications: malnutrition, portal hypertension
- Medical treatment (supportive care, anti-coagulation, thrombolysis).
- Anticoagulants are used to prevent the extension of the thrombus and the body deals with the already formed thrombus by the fibrinolytic activity of the blood and the forming of the collaterals.
- If that failed, we go to radiologic procedures (angioplasty, TIPS,) If that failed, we go to Surgical intervention (shunting procedures, transplantation).
A. Medical therapy
Management of the original disease:
- If the patient was taking oral contraceptive pills, she must stop them.
- If the patient comes with ascites, we should manage symptomatically as he should: Diuretics, low sodium diet, and LVP.
- If the patient develops hematemesis, we do an upper GIT endoscopy and manage the bleeding.
- Improve nutritional status.
- The myeloproliferative disorder may benefit from treatment with aspirin and hydroxyurea.
- Anticoagulation alone is unlikely to lead to sufficient recanalization of occluded vessels to avoid the progression of liver disease.
- A trend for a benefit of anticoagulation on survival in less severe disease.
- Anticoagulation therapy, We start with Low molecular weight heparin and then continue with oral anticoagulant.
- Used in: Chronic or subacute Budd-Chiari syndrome with well-compensated liver disease at the time of presentation. When other types of therapy are not Feasible.
B. Radiologic treatment
If the patient gives response to the therapy and is well-controlled we don’t go to these procedures.
- Angioplasty (we set a stent to restore the patency of the occluded blood vessel). Angioplasty has some criteria according to the size and the number of the segments that have been occluded, the certain blood vessels, the duration of the occlusion whether recent or long duration and the type of the thrombus whether malignant or benign.
- Stenting.
- TIPS.
C. Surgical therapy
Failed or not accessible radiologic treatment we go to surgical therapy.
- Restore hepatic venous drainage using shunt surgery.
- Because of the availability of TIPS, few vascular surgeons routinely perform shunt surgery.
- Underlying cause of the thrombotic diathesis (tendency) should be identified and treated prior to considering shunt surgery.
- Unlikely to be beneficial in patients who have cirrhosis, such patients are best managed with liver transplantation.
D. Liver transplantation
- To whom are not candidates for radiologic or surgical decompression or who have decompensated cirrhosis.
- Protein S, protein C, or antithrombin III deficiency may also be cured of their clotting tendency by liver transplantation.
- Survival following OLT (orthotopic liver transplantation) depends upon the underlying cause of the Budd-Chiari syndrome and the patient’s condition at the time of the transplant.
- There are 2 types of liver transplantation: cadaver donor as we take the whole liver from has just died and living donor as we take half of the liver.
- In autoimmune hepatitis if the patient comes late in acute or chronic liver failure, it is too late to restore the patency of the blood vessels as the organ has already failed so I go to liver transplantation.
- In autoimmune-related liver failure or Budd-Chiari if the patient came in a cold state means (decompensated cirrhosis or chronic liver failure) he has the time to bring a living donor but if he came with (acute liver failure) there is no time so he takes cadaveric liver transplantation.
Portal vein thrombosis
There are a lot of similarities between Budd-Chiari syndrome and portal vein thrombosis. If we talk about portal vein thrombosis, we mean benign but there is also malignant or tumorous portal vein thrombosis.
Local causes: The portal vein drains the whole GIT, if there is inflammation or trauma or surgery of any organ of the GIT that will cause portal vein thrombosis.
Generalized causes: The same as the examples of thrombophilia of portal vein thrombosis.
Local Risk Factors for Portal Vein Thrombosis
- Cancer (malignancy of GIT or of liver such as HCC).
- Neonatal omphalitis, umbilical vein catheterization.
- Preserved liver function with precipitating factors (splenectomy, surgical portosystemic shunting, TIPS dysfunction, thrombophilia).
- Advanced disease in the absence of obvious precipitating factors.
Other risk factors
Affection of Any abdominal organ:
- Diverticulitis.
- Appendicitis.
- Pancreatitis.
- Duodenal ulcer.
- Cholecystitis.
- Crohn’s disease, Ulcerative colitis.
- Tuberculous lymphadenitis.
- Cytomegalovirus hepatitis.
- Injury to the portal venous system.
Trauma of the blood vessels during surgery:
- Splenectomy.
- Colectomy, Gastrectomy.
- Cholecystectomy.
- Surgical portosystemic shunting, TIPS, Liver transplantation.
- The trauma of the blood vessels and causes injury of the intima of the blood vessel and predisposes it to the rough intima which causes portal vein thrombosis.
Cirrhosis:
- Cirrhosis is the most common cause and the major etiological factor of portal vein thrombosis.
- Portal vein thrombosis is differentiated into cirrhotic and non-cirrhotic as it is different in management as the cirrhotic patient has liability for bleeding and the presence of varices.
Clinical picture
Abdominal pain. So portal vein thrombosis is a differential diagnosis of abdominal pain especially in patients who don’t respond or have risk factors or patients with hematemesis.
Manifestations of bowel ischemia (diarrhea or bloody diarrhea). If there is an extension of the thrombus to the mesenteric vein.
Diagnosis
The diagnosis is the same as Budd-Chiari, we use Doppler but on the portal vein to detect the patency and the development of collateral circulation, recently developed thrombus or chronic (old) thrombus and whether the patient is cirrhotic or not as the management differs. To confirm the diagnosis, we use CT or MRI angiography (portography).
Treatment
- Start to manage the original disease, The management differs if it is acute (recently thrombus) or chronic (old thrombus), and if it is cirrhotic or non-cirrhotic patient.
- In acute (recent thrombus) and non-cirrhotic patients: the mainstay treatment is anti-coagulation therapy, later if it fails, we use interventional radiological procedures.
- If the cirrhotic patient with chronic thrombus.
- here we measure the risks and and if there is a risk of bleeding or if there are collaterals or not and there is a debate if we will use the oral anticoagulants (anti-coagulation therapy) or not.
You can subscribe to science online on YouTube from this link: Science Online
You can download the Science Online application on Google Play from this link: Science Online Apps on Google Play
Vascular Liver Disorders, Causes and risk factors of Budd-Chiari syndrome
Autoimmune Hepatitis symptoms, types, diagnosis, causes and treatment
Primary biliary cirrhosis symptoms, cause, diagnosis, treatment, and Osteoporosis
Diagnosis of the cause of jaundice, Hepatobiliary imaging, treatment of cholestasis and Pruritus
Liver Cholestasis types, causes, features, symptoms, diagnosis, and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer