Minimal HE (MHE), minimal hepatic encephalopathy symptoms, diagnosis, test and Treatment
The presence of test-dependent or clinical signs of brain dysfunction in patients with CLD (chronic liver disease) who are not disoriented or display asterixis, Patients with MHE tend to develop overt HE, MHE impairs health-related quality of life, patient’s ability to work and daily function including driving skills with increased incidence of car accidents.
Minimal HE (MHE)
Patients with MHE will by time turn to be manifest encephalopathy. Liver transplantation should be considered in patients with MHE, The areas with impairments are attention, visual perception, speed of information processing, fine motor skills, and short-term memory.
How to test for MHE? (We test for it by Psychomotor tests)
1) Critical flicker frequency (CFF)
- A diagnostic bedside test for MHE.
- It measures visual discrimination and general arousal.
- Patients are first instructed and trained about the procedure.
- Measurement of CFF thresholds is done by intrafoveal stimulation with a luminous diode.
- Decreasing the frequency of the light pulses from 60 Hz downward, the CFF threshold is determined as the frequency when the impression of fused light turned to be a flickering one.
- The critical flicker frequency (CFF) threshold is defined as the frequency at which a flickering light is indistinguishable from a steady, non-flickering light.
2) Stroop test
Evaluates selective attention and processing speed by the interference between visual color and a written color name.
3) Inhibitory Control Test (ICT)
- A computerized test that evaluates sustained attention and working memory impairment.
- During the ICT, which takes about 15 minutes, subjects see a continuous stream of letters on a computer screen and they are instructed to hit a button if they see an X followed by a Y; the test utilizes lures (XX or YY) to evaluate the ability of the subject to inhibit the response to the lures.
- The test is scored based on the number of correct responses to targets and the lure rate.
4) Psychometric Hepatic Encephalopathy Score (PHES)
Utilizes a subset of five tests. This test primarily evaluates attention, visuospatial perception, visuospatial construction, psychomotor speed, and motor accuracy. These tests were used in the past but still, we can use them because some of them are very simple tests. The five tests consist of:
- Number Connection Test A.
- Number Connection Test B.
- Line Tracing test.
- Digit Symbol Test.
- Serial Dotting Test
In the number connection test, the patient is asked to connect the numbers and we will find the motor skills of this patient, In the Line Tracing Test, the patient is asked to pass through this line without going out of it
5) Continuous Reaction Time (CRT) test
The CRT index test measures the stability of motor reaction time (pressing a button as a response to auditory stimuli) and requires simple software and hardware to administer.
6) SCAN Test
The SCAN Test measures speed and accuracy of a digit recognition memory exam in a computerized format.
Some of these tests can be used even by the patient himself for self-assessment by applying them to his mobile phone.
Blood ammonia
Increased blood ammonia alone does not add any diagnostic, staging, or prognostic value for HE in patients with CLD, A normal value calls for a diagnostic reevaluation, However, for ammonia-lowering drugs, repeated measurements of ammonia may be helpful to test the efficacy and to stop the drugs.
For example, if you have a patient with a coma and you’re suspecting HE and the patient has a normal blood ammonia level, you must reevaluate this patient again for possible causes rather than HE.
However, other patients with no acute or chronic liver disease may have elevated blood ammonia without HE such as drugs as Valproic acid and other drugs may lead to HE and other congenital anomalies related to the urea cycle and many other causes of elevated blood ammonia without the presence of chronic liver disease.
Management of HE
Exclude non-hepatic causes of altered mentation.
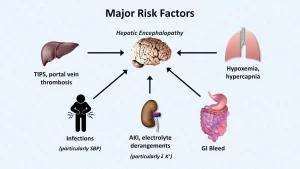
Identify and correct the precipitating factor is of paramount importance, because nearly 90% of patients can be treated with just correction of the precipitating factor:
- Hypovolemia: some ascites or edema are better than HE.
- Hyponatremia and electrolyte imbalance.
- Sepsis.
- Drugs.
- High protein diet.
- GIT bleeding.
- Constipation.
- Concomitant disorder (anemia, alcohol intake).
Differential diagnosis of HE
Acute confusional state
- Diabetic complications (hypoglycemic attacks may induce a disturbance in the level of consciousness).
- Alcohol (intoxication, withdrawal, Wernicke).
- Drugs (benzodiaz, opioids).
- Neuroinfections.
- Electrolyte disorders (Na, Ca).
- Nonconvulsive epilepsy.
- Psychiatric disorders.
- Intracranial bleeding, stroke.
Other presentations
- Dementia (primary and secondary).
- Brain lesions (traumatic, neoplasms, normal pressure hydrocephalus).
- Obstructive sleep apnea.
- Hyponatremia and sepsis.
- Uremic encephalopathy.
Treatment of HE
The most important differential diagnosis of HE is hypoglycemia, The definite treatment of HE is liver transplantation, and once the patient developed HE, transplantation is indicated.
1. Diet
65-90% of cirrhotics have malnutrition and incidence of HE, Protein restriction is controversial. (Some allow the patients to take protein freely, others will restrict them, especially in attacks of acute encephalopathy). Much protein restriction should be avoided to maintain a positive nitrogen balance.
Non-animal protein might be better. (White meat is better than red meat), Modify the composition of the diet to increase the caloric/nitrogen ratio. High fiber diet is preferred. (it’s associated with decreased clearance time of the fecal content from the gut and avoidance of constipation and hypoglycemia).
2. Enema
3. Lactulose (nonabsorbable disaccharide)
- The standard of care treatment for HE over 30 ys.
- Mechanism: lactulose → lactate + acetate.
- Dose: 15-30 CC oral 1-3 times daily.
- FDA approval in the treatment of HE.
- S E: bloating, colics, sweet taste, and diarrhea.
4. Neomycin (mainly locally acting aminoglycoside antibiotic)
Mechanism: affect the intestinal flora to generate ammonia, Dose: 3-6 gm/d oral in the first 3 days then, 1-2 gm/d thereafter, FDA approval in the treatment of HE, S E: systemic absorption up to 4 % → possible nephrotoxicity and ototoxicity.
5. Rifaximin
- A minimally-absorbable gut-selective rifamycin derivative with antibiotic activity against enteric aerobic and anaerobic microorganisms (which are important sources of ammonia).
- Being minimally absorbable (< 0.4%) allows it to reach high concentrations in the intestinal tract and to remain in the feces in its
- active form with minimal systemic side effects.
- Concentration: 200 or 550 mg oral tablets.
- Administration: 400 mg tds or 550mg bid.
- SE:
- Nausea, vomiting, abdominal pain.
- Flatulence, diarrhea, tenesmus.
- Headache.
- Increase in S. Na and K.
- Long-term therapy may impair the already altered clotting status due to the reduction of E coli in the gut.
Rifaximin and prophylaxis of HE
It is recommended that patients with a history of recurrent acute HE should be maintained on rifaximin ± lactulose to reduce the risk of recurrent HE and related hospitalization.
6. Flagyl (Metronidazole)
- Dose: 500 mg three times daily.
- Mechanism: affects intestinal flora.
- SE: metallic taste, anorexia, and peripheral neuropathy.
- Can be used as an alternative to antibiotics.
7. L-ornithine L-aspartate (LOLA): I.V and oral forms
Both i. v and oral forms significantly reduced blood ammonia levels in patients with HE. LOLA is a compound salt that stimulates ornithine transcarbamoylase and carbamoyl phosphate synthetase in the liver and is a substrate for the formation of urea. LOLA also stimulates glutamine synthesis in skeletal muscle and consequently lowers ammonia concentration.
LOLA has been most thoroughly evaluated in the setting of chronic HE. Randomized, placebo-controlled, double-blind studies were performed in Germany using an intravenous and an oral form of LOLA in patients with chronic HE, both of which demonstrated improvements in the number of connection tests, ammonia values, and HE parameters (mental state gradation and Portosystemic Encephalopathy Index).
8. Branched-chain amino acids: IV and oral forms.
9. Flumazenil IV form; benzodiazepine receptor antagonist.
10. Zinc.
11. L-dopa and bromocriptine.
12. Probiotics
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Hepatorenal syndrome (HRS) risk factors, diagnosis, symptoms, types, causes and treatment
Refractory ascites symptoms, cause, types and treatment of refractory ascites in cirrhosis
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Liver Cirrhosis causes, symptoms, treatment & stages, Liver Biopsy and treatment of PHTN
Viral hepatitis, HDV symptoms, Treatment of acute HCV, Occult hepatitis C and HEV
Acute Hepatitis Causes, Diagnosis, and Treatment, Chronic hepatitis and Liver biopsy
Liver development, congenital anomalies, function & Pancreas development