Life cycle of varicella zoster virus, Cytomegalovirus and Diagnosis of Infectious mononucleosis
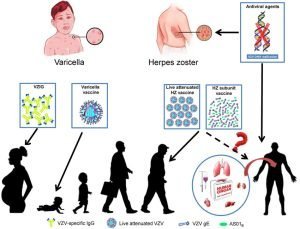
VZV causes chickenpox (varicella) and, on recurrence, causes herpes zoster, or shingles, Varicella is a mild, highly contagious disease, chiefly of children, characterized clinically by a generalized vesicular eruption of the skin and mucous membranes. The disease may be severe in adults and immunocompromised individuals.
Varicella Zoster Virus
Herpes zoster is a sporadic, incapacitating disease of elderly or immunocompromised individuals that is characterized by pain and vesicular rash limited in distribution to the skin innervated by a single sensory ganglion, The lesions are similar to those of varicella, Varicella is the acute disease that follows primary contact with the virus, while zoster is the response of the partially immune host to reactivation of the varicella virus present in latent form in neurons in sensory ganglia.
Pathogenesis and Immunity
VZV is spread principally by airborne droplets and by direct contact with skin vesicles, Primary infection begins in the tonsils and mucosa of the respiratory tract, After initial replication in regional lymph nodes, the virus progresses via the bloodstream and the lymphatic system to the liver and spleen.
Secondary viremia spreads the virus throughout the body and to the skin, where the typical rash develops, Virus replication in the lung is a major source of spread to other hosts, Following primary infection, VZV becomes latent in the dorsal root, cranial nerve, and other ganglia, It can be reactivated in older adults when immunity wanes or in patients with impaired cellular immunity.
On reactivation, the virus replicates and is released along the length of the neuron to infect the skin, causing a vesicular rash along the entire dermatome, which is known as herpes zoster, or shingles. This damages the neuron and may result in painful postherpetic neuralgia.
Life cycle of varicella zoster virus (VSV)
Previous infection with varicella is believed to confer lifelong immunity to varicella, Herpes zoster occurs in the presence of neutralizing antibodies to varicella, The development of varicella-zoster virus-specific cell mediated immunity is important in the recovery from both varicella and zoster.
A live attenuated vaccine for VZV (Varivax) is available, it is administered after 1 year of age and induces the production of protective antibodies and cell-mediated immunity, A stronger version of this vaccine (Zostavax) is available for adults older than 50 years, It is effective in at reducing both the frequency of outbreaks of zoster and the severity of the disease.
Epstein bear virus
EBV is ubiquitous with a herpesvirus with a limited host range and tissue tropism. It is the causative agent of acute infectious mononucleosis and has been causally associated with nasopharyngeal carcinoma, Burkitt lymphoma, Hodgkin and non-Hodgkin lymphomas, other lymphoproliferative disorders in immunodeficient individuals, and gastric carcinoma, The major target cell for EBV is the B lymphocyte, Some epithelial cells of the oropharynx and nasopharynx also express the viral receptor.
Pathogenesis and Pathology
A. Primary Infection
It is transmitted by infected saliva and initiates infection in the oropharynx, Viral replicates in epithelial cells (or surface B lymphocytes) of the pharynx and salivary glands, Infected B cells spread the infection from the oropharynx to lymphatic tissue and blood. Normally most virus-infected cells are eliminated, but small numbers of latently infected B lymphocytes persist for the lifetime of the host.
In children, 1ry infections are usually subclinical, but in young adults, acute infectious mononucleosis often develops, Mononucleosis is a polyclonal stimulation of lymphocytes. The classic lymphocytosis and swelling of lymphoid organs (lymph nodes, spleen, and liver, associated with infectious mononucleosis results mainly from the activation and proliferation of T cells.
T cells are essential for limiting the proliferation of EBV-infected B cells and controlling the disease, EBV-infected B cells synthesize immunoglobulin, Most patients develop transient heterophil antibodies that agglutinate sheep, horse, and bovine erythrocytes.
B. Reactivation from Latency
EBV may be reactivated when the memory B cell is activated (especially in the tonsils or oropharynx) and may be shed in saliva, Reactivations are usually clinically silent, and Immunosuppression is known to reactivate infection, sometimes with serious consequences.
Clinical Findings
Most primary infections in children are asymptomatic. In adolescents and young adults. the classic syndrome associated with primary infection is infectious mononucleosis, EBV is also associated with several types of cancer.
A. Infectious Mononucleosis (Heterophile Antibody-Positive Infectious Mononucleosis)
The triad of classic symptoms for infectious mononucleosis is lymphadenopathy, splenomegaly, and exudative pharyngitis accompanied by high fever, malaise, and fatigue. Some patients develop signs of hepatitis. The typical illness is self-limited for 2-4 weeks. During the disease, there is an increase in the number of circulating white blood cells, with a predominance of lymphocytes, Many of these are large, atypical T lymphocytes.
B. Cancer
EBV-associated Burkitt lymphoma, nasopharyngeal carcinoma, Hodgkin and non-Hodgkin lymphomas, and gastric carcinoma, EBV-associated posttransplant lymphoproliferative disorders are a complication for immunodeficient patients.
Laboratory Diagnosis of Infectious mononucleosis
1- Blood smears: The finding of atypical lymphocytes and the presence of lymphocytosis.
2-Serology:
- Detection antibody to viral antigens. The presence of antibodies of the IgM type is indicative of current infection while antibody of the IgG type is a marker of past infection and indicates immunity. Common serologic procedures for the detection of EBV antibodies include enzyme-linked immunosorbent assays, immunoblot assays, and indirect immunofluorescence tests.
- The heterophile antibody (Monospot) test: The less specific heterophil agglutination test may be used to diagnose acute EBV infections.
3- Detection of viral nucleic acid using PCR NA probes is the most sensitive means of detecting EBV in blood, body fluids, and tissues.
Treatment, prevention, and control
No effective treatment or vaccine is available for EBV disease, Acyclovir will reduce viral shedding but has no effect on the disease, The ubiquitous nature of the virus and the potential for asymptomatic shedding make control of infection difficult.
Cytomegalovirus
CMV is a ubiquitous herpesvirus that is a common cause of human disease, CMV is the most common cause of congenital infection which can lead to severe abnormalities, Although, usually a mild or asymptomatic disease in children and adults, CMV is particularly important as an opportunistic pathogen in immunocompromised patients.
Pathogenesis
Humans are the only known host for CMV. The virus replicates fibroblasts, epithelial granulocytes, and macrophages and establishes latency in hematopoietic progenitor cells in the bone marrow and monocytes.
CMV may be shed in urine, saliva, semen, breast milk, and cervical secretions and is carried in circulating white blood cells, Transmission from person to person thus occurs in different ways, via the congenital, oral, and sexual routes, blood transfusion, and tissue transplantation.
Clinical Findings
A. Normal Hosts
Primary CMV infection of older children and adults is usually asymptomatic but occasionally causes heterophile-negative mononucleosis syndrome. CMV mononucleosis is a mild disease, and complications are rare.
B. Immunocompromised Hosts
Both morbidity and mortality rates are increased with primary and recurrent CMV infections in immunocompromised individuals, The virus may be restricted to a single organ, causing pneumonia colitis, retinitis or hepatitis, or cause disseminated infection, CMV is also responsible for CMV-related rejection of renal allografts In untreated AIDS patients; colitis and chorioretinitis are common problems, the latter often leading to progressive blindness.
C. Congenital and Perinatal Infections
Fetal and newborn infections with CMV may be severe, The virus can be transmitted in utero with both primary and reactivated maternal infections, Generalized cytomegalic inclusion disease results most often from primary maternal infections, The name derives from the tendency for massive enlargement of CMV-infected cells with intranuclear inclusion bodies.
Clinical features include intrauterine growth retardation jaundice, hepatosplenomegaly, thrombocytopenia, microcephaly, and retinitis, CMV is the most common infectious cause of congenital hearing loss, vision loss, and mental retardation are also common consequences of congenital CMV infection.
Laboratory diagnosis
- Antigen Detection Assays: Monoclonal antibodies against viral antigens can be used to detect CMV antigens in peripheral blood white cells by the indirect immunofluorescent technique. The test provides a sensitive and specific prediction of disease activity.
- Genome detection: PCR assays are used to detect the circulating virus in the blood, CSE, and urine PCR assays can provide quantitative viral load data which can be used to predict CMV disease in immunocompromised patients.
- Culture: Human fibroblasts are used for the isolation of CMV, In cultures. CPE develops slowly, consisting of small foci of swollen cells with large intranuclear inclusions.
- Serology: Many types of assays can detect CMV antibodies, Seroconversion is usually an excellent marker for primary CMV infection Serologic assays are not informative for immunocompromised patients.
Treatment and Control
Ganciclovir, valganciclovir, cidofovir, and foscarnet have been approved for the treatment of life-threatening CMV infections in immunosuppressed patients. Ganciclovir is structurally similar to acyclovir, it inhibits viral DNA polymerase. Cidofovir and foscarnet can be used for the treatment of CMV retinitis and for ganciclovir-resistant CMV strains.
Human herpes virus 6, Human herpes virus 7
HHV-6 and HHV-7 are T-lymphotropic viruses. Both primarily infect lymphocytes, especially CD4 T cells and establish a latent infection in hematopoietic progenitor çells. Infection by these viruses occurs early in life, and transmission is via saliva and secretions. Primary infection with HHV-6 or HHV-7 has been linked with exanthem subitum (roseola infantum or Sixth disease in infants and young children.
Human herpes virus 8
HHV-8, also known as Kaposi sarcoma-associated herpes virus (KSHV) is not as ubiquitous as other herpesviruses. Usually, infection with HHV-8 is associated with AIDS patients. KSHV is the cause of Kaposi sarcomas; a vascular tumour of skin, lymph nodes, and visceral organs. The virus is most likely spread via oral secretions, but may be spread by other means (sexually, vertically, by blood, and through organ transplants).
You can follow science online on YouTube from this link: Science online
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Herpesviruses structure, types, Herpes simplex viruses, Genital Herpes & Skin Infections
Vaccines types, Live vaccines, Inactivated vaccines, Subunit vaccines, Naked DNA & mRNA vaccines
Adaptive (Acquired immunity) types, Difference between Innate & Adaptive Immune responses
Features and classification of viruses, Defective viruses & Viral vectors used for gene therapy
Cytokines function, use, definition, inflammation & side effects