Carbohydrate Metabolism, Importance and Hormonal regulation of glycolysis
Carbohydrates are composed of carbon, hydrogen, and oxygen atoms, The family of carbohydrates includes both simple and complex sugars. Glucose & fructose are examples of simple sugars, and starch, glycogen, and cellulose are all examples of complex sugars. The complex sugars are called polysaccharides and they are made of multiple monosaccharide molecules.
Carbohydrate metabolism
Carbohydrate metabolism is responsible for the metabolic formation, breakdown, and interconversion of carbohydrates in living organisms, It ensures a constant supply of energy to the living cells, The most important carbohydrate is glucose, glucose can be broken down via glycolysis, It enters into the Kreb’s cycle & oxidative phosphorylation to generate ATP.
Fates of the absorbed monosaccharide
Glucose, fructose, galactose, and other monosaccharides are absorbed through portal blood to the liver. Fructose is either oxidized or converted to glucose in the liver, while galactose is converted to glucose. The only sugar circulates in the blood is glucose. Part of this glucose is used in the liver to be stored as glycogen, oxidized or used in lipid synthesis. Another part passes through systemic circulation to maintain blood glucose level (the fasting blood glucose level 70-110 mg/dl).
Glucose is used intracellular in:
Oxidation: The pathways for oxidation of glucose are:
- Major pathways, which are mainly for energy production: Glycolysis, followed by oxidative decarboxylation of pyruvate and citric acid cycle (CAC).
- Minor pathways, which are not for energy production: Hexose monophosphate shunt (HMS) and Uronic acid pathway.
Conversion to biologically active substances as:
- Galactose: This is essential for the formation of lactose, glycolipids, mucopolysaccharides, etc.
- Fructose: needed for the nutrition of sperms.
- Amino sugars.
- Non-essential amino acids.
- Fatty acids.
- Ribose-5-P.
- Glucuronic acid.
Storage of glucose as:
- Glycogen in the liver and muscles mainly.
- Triglycerides (TG), mainly in adipose tissues.
Excretion of glucose in urine: When blood glucose level exceeds the renal sugar threshold (180 mg/dl), it passes to urine. This is known as glucosuria.
Glycolysis (Embden Meyerhof pathway)
It is the degradation of glucose to generate ATP and to provide intermediates for other synthetic and metabolic pathways. Aerobically it ends with pyruvate while anaerobically lactate is the end product.
Site of glycolysis
It occurs in the cell cytosol of all tissues. It is the principle route for glucose metabolism and the main pathway for the metabolism of fructose and other carbohydrates derived from the diet.
Steps of glycolysis
Conversion of glucose to G-6-P by hexokinase or glucokinase.
Importance of glycolysis
Energy production:
Under aerobic conditions: Glucose → 2 pyruvate + 8 ATP
For tissues that have mitochondria, glycolysis is considered a preparatory step for complete oxidation via the citric acid cycle. The hydrogens of NADH produced by glycolysis are transported to the mitochondria to be oxidized by electron transport chain (ETC).
Under anaerobic conditions: Glucose → 2 lactate + 2 ATP
Pyruvate is reduced to lactate in a reversible reaction catalyzed by lactate dehydrogenase (LDH). This reaction provides oxidized NAD to insure the continuation of the pay off phase of glycolysis and production of the 4 ATP molecules at the substrate level.
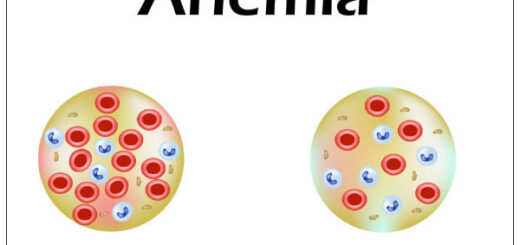
This occurs in muscles during severe exercise, and hypoxic conditions, and in tissues that lack mitochondria as RBCs and lens. The decrease in the amount of O2 will necessitate an increase in anaerobic glycolysis for the energy production, leading to the generation of a large amount of lactic acid. Lactic acid diffuses to the circulation and taken by:
- The liver to enter the gluconeogenic pathway that provides glucose to the blood that partially compensates the high rate of anaerobic glucose oxidation.
- The heart that converts lactate to pyruvate which is used for energy production.
- Kidney to be excreted in the urine.
Cori cycle: Lactate which is formed during anaerobic oxidation of glucose in muscles and in RBCs diffuses to the blood then to the liver. In the liver, lactate can be converted to glucose by gluconeogenesis, Glucose goes back to tissues and is reutilized for the production of energy.
Synthetic functions of glycolysis
- Dihydroxyacetone phosphate can give glycerol-3-phosphate for the synthesis of TAG and phospholipids.
- Pyruvate→ acetyl coA → FA and sterols
- Synthesis of amino acids from intermediates of glycolysis.
Importance of glycolysis in red cells
- Energy production is the only pathway that supplies the red cells with ATP. Since red cells are dependent on glycolysis for the production of ATP, some types of hemolytic anaemias are due to an inherited deficiency of glycolytic enzymes mainly pyruvate kinase deficiency.
- Reduction of methemoglobin: glycolysis provides NADH for the reduction of met Hb by NADH-cytb5-reductase enzyme.
- In red cells, 1,3 bisphosphoglycerate is converted to 2,3 bisphosphoglycerate which binds to oxy Hb decreasing its affinity to O2 and helps the release of oxygen at tissues.
Regulation of glycolysis
The rate of glycolysis is regulated by the activity of the three irreversible enzymes, hexokinase, PFK, and pyruvate kinase. PFK is the main pacemaker, since it catalyzes the first irreversible reaction unique to the glycolytic pathway (the committed step). PFK is allosterically inhibited by high levels of ATP (high energy state of the cell) and citrate (substrate feedback inhibition). It is allosterically activated by elevated levels of AMP (low energy state of the cell), and F-6-phosphate (substrate activation).
Hormonal regulation of glycolysis
Glucagon is secreted in hypoglycemia or in carbohydrate deficiency. It affects liver cells mainly as follows:
- It acts as a repressor of glycolytic key enzymes (glucokinase, PFK-1, pyruvate kinase).
- It produces phosphorylation of specific enzymes leading to the inactivation of glycolytic key enzymes.
Insulin is secreted in hyperglycemia and after carbohydrates feeding, it causes:
- Induction for the synthesis of glycolytic key enzymes.
- Activation of glycolytic key enzymes.
Regulation is achieved through hormones (induction or repression of the regulated enzymes and covalent modification) and allosteric modifiers
Inhibitors of glycolysis
- Mercury and iodoacetate inhibit glyceraldehyde-3-P dehydrogenase by binding to a thiol (SH) group in its active site.
- Fluoride inhibits enolase by the removal of Mg2+ as Mg fluoride.
Arsenate is an uncoupler of oxidation and phosphorylation, it forms 1-areseno-3-phosphoglycerate which interferes with ATP formation at a substrate level, but it does not prevent flux through glycolysis. Arsenate competes for inorganic phosphate binding sites on enzymes, resulting in the formation of arsenate esters which are unstable.
Pyruvate is transported to the mitochondria via a special pyruvate transporter where it can be transformed into Acetyl Co-A by oxidative decarboxylation catalyzed by a multi-enzyme complex known as pyruvate dehydrogenase complex. This reaction needs five cofactors which are: thiamine pyrophosphate (TPP or active vitamin B1), lipoic acid (L), coenzyme A (CoASH) FAD and NAD+. It provides extra 6 molecules of ATP formed by oxidation of 2 molecules NADH by the ETC.
Regulation of the activity of the pyruvate dehydrogenase complex
- Acetyl CoA and NADH+H+ (the products of oxidation of pyruvate), allosterically inhibit the enzyme complex.
- Covalent modification. The enzyme exists in active dephosphorylated form and it is inactive in phosphorylated form.
Arsenite and mercury inhibit pyruvate dehydrogenase complex by reacting with the sulphhhydryl group of lipoic acid leading to the accumulation of pyruvate and the formation of lactic acid & lactic acidosis.
Cellular respiration, Structure of ATP and types of fermentation
Functions of Lymphatic system, Structure of Lymph nodes, Spleen & Tonsils
Lymphatic system structure, Function of Thymus, Vascular supply & blood-thymus barrier
Immune system structure, function, cells & Types of body defense mechanisms