Intestinal motility, Intestinal movements types and Factors affecting Rate of intestinal absorption
The movements of the small intestine mix the intestinal contents and propel them toward the large intestine, Contractions of the small intestine are coordinated by the basic electric rhythm, enteric nervous system, extrinsic autonomic nerves, and GIT hormones.
Intestinal motility
The rate of the BER is about 12/min in the duodenum and falls to about 8/min in the distal ileum, In the colon, the BER rate rises from about 2/min at the cecum to about 6/min at the sigmoid, When a meal is ingested, the MMCs that pass along the intestine at regular intervals in the fasting state are replaced by other types of intestinal contractions.
Types of intestinal movements
There are mainly 2 movements: Segmenting (mixing) and peristaltic (propulsive).
1. Segmenting movements (mixing contractions)
- Segmentation of the small intestine occurs in response to distension with chyme, They are ring-like contractions dividing a loop of the intestine into equal portions, giving the appearance of a chain of sausages, Then, these contractions relax and a new set of contractions begin in the previously relaxed points.
- The maximum frequency of the segmentation contractions in the small intestine is determined by the frequency of the basic electrical rhythm, So, they occur at a rate of 12/minute in the duodenum and decrease to 8/minute in the terminal ileum.
- Although slow waves in the smooth muscle cause the segmentation contractions, these contractions are ineffective without background excitation mainly from the myenteric nerve plexus.
- Segmentation mixes the intestinal contents with the digestive juices, moves the chyme to and fro, and increases its exposure to the mucosal surface, Also, it slows transit in the small intestine to permit longer contact of the chyme with the enterocytes and fosters absorption.
2. Peristaltic movements (propulsive movements).
- Peristalsis is a reflex response that is initiated when the gut wall is stretched by the contents of the lumen, and it occurs in all parts of the gastrointestinal tract from the esophagus to the rectum.
- The stretch of the duodenal wall initiates a circular muscle contraction behind the stimulus and an area of receptive relaxation in front of it. The wave of contraction then moves in an oral-to-caudal direction, propelling the contents of the lumen forward.
- Peristalsis is an excellent example of the integrated activity of the enteric nervous system, It appears that local stretch releases serotonin, which activates the myenteric plexus, Then, impulses pass in a retrograde direction in this plexus to activate the release of substance P and acetylcholine, causing circular smooth muscle contraction, At the same time, impulses passing in an anterograde direction activate the secretion of NO, VIP, and adenosine triphosphate (ATP), producing the relaxation ahead of the stimulus.
- In addition to the stretch of duodenum, the peristaltic activity of the small intestine could be initiated by the gastroenteric reflex: Distention of the stomach excites some receptors and this reflex is carried out by the myenteric plexus from the stomach down along the wall of the small intestine.
- Peristalsis promotes the propulsion of food through the small intestine, The movement of food along the small intestine normally averages only 1 cm/min, Which means that 3 to 5 hours are required for the passage of chyme from the pylorus to the ileocecal valve.
- Peristaltic movements lead to the forward movement of food toward the ileocecal valve and spread out of chyme along the intestinal mucosa.
Segmenting movements have some propulsive effect, and peristalsis has some mixing effect.
3. Antiperistalsis
This is a peristalsis in opposite direction, i.e.
- Between duodenum and stomach: to allow time for neutralization.
- Between ileum and coecum; to allow time for absorption.
4. MMC
In the period between meals, the intestine is relatively quiescent, but every 90 min or so it is swept through by a large peristaltic wave triggered by the hormone motilin.
Peristaltic rush: is a powerful series of peristaltic waves that travel along the small intestine in a few minutes, It occurs in some infectious diseases, i.e. it is not present in normal conditions, The peristaltic rush takes the intestinal contents toward the colon to get rid of any distention or irritation.
Regulation of Intestinal movements
I- Nervous regulation
Intestinal movements are not dependent on extrinsic nerves, and can continue without them, However, the vagus and splanchnic nerves regulate the frequency and magnitude of the BER and so the intestinal movements.
Innervation of the small intestine
- Parasympathetic supply: is via the vagus nerves which are motor to the wall, but inhibitory to the sphincter.
- Sympathetic: is via the splanchnic nerves which are inhibitory to the wall and motor to the sphincters.
During rest, the small intestine is inhibited by a strong inhibitory sympathetic tone, The ileocecal sphincter is supplied by motor sympathetic fibers, which keeps the sphincter closed by tonic contraction to prevent backflow from the caecum to the ileum, The presence of vagal inhibitory fibers in this valve is doubtful.
II- Hormonal regulation
Gastrin, CCK, insulin, motilin, and serotonin, all enhance intestinal motility, Conversely, secretin and glucagon inhibit small intestinal motility
Absorption
Absorption is the transfer of digestive products from the lumen of the small intestine to the bloodstream, through the mucosal cells.
The total quantity of fluid that must be absorbed from the small intestine each day is equal to about 2 liters of ingested fluid plus about 7 liters of gastrointestinal secretions secreted per day; only about 1500 ml pass through the ileo-colic valve daily.
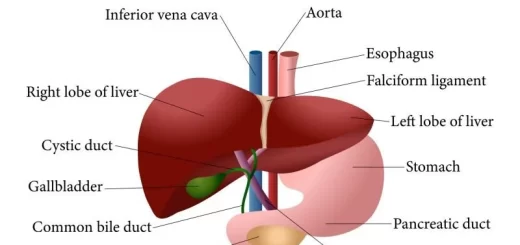
The large intestine can absorb water and electrolytes, The stomach is a poor absorptive area of the gastrointestinal tract, Only a few highly lipid-soluble substances, such as alcohol and some drugs, can be absorbed in small quantities, The great absorbing power of the small intestine is due to:
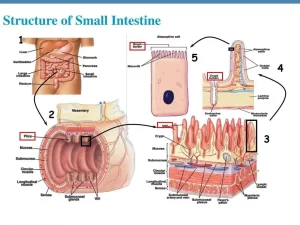
- Long absorbing surface (280 cm in the living human).
- Rich blood and lymphatic vessels supply.
- The presence of intestinal villi which increase the absorptive surface area 10-folds, and the protrusion from each cell of the intestinal mucosa of microvilli which increase the surface area another 20-fold.
The intestinal villi
Throughout the small intestine, it is folded up into fingerlike projections called villi. They are lined with columnar epithelial cells characterized by extensive microvilli at their apical membranes. the “central lacteal. In the center of each villus, there is a club-shaped lymph capillary, called the ”central lacteal”.
Chylomicrons are absorbed in these lacteals, which drain their lymph into lymph plexuses in the intestinal wall and then into the thoracic duct to the venous system. Along the lymph plexuses, there are valves that allow the flow of lymph only in one direction, into the thoracic duct to the venous blood.
Each villus is supplied with one or two arterioles, and is drained by two venules. Monosaccharides and amino acids are absorbed in the tributaries of the portal vein to the liver, and then they are passed to the systemic circulation.
Movements of the villi
The villi show continuous movements during absorption, the villi act as pumps, they shorten and squeeze the blood and lymph, and then elongate to imbibe more intestinal contents. The villi also show side-to-side movements. These movements of the villi facilitate the contact of enterocytes with the intestinal contents in the lumen, to enhance digestion and absorption.
Villikinin
It is a local hormone, released by intestinal mucosa when it comes in contact with the digestive products of food. It stimulates movement of the villi and aids absorption.
Factors affecting the rate of intestinal absorption
Any factor which affects the metabolic activity of the intestinal mucosa reflects itself on intestinal absorption, Also, Physico-chemical factors affect it.
- Viability of the intestinal mucosa: An adequate blood flow, oxygen supply, and the general metabolic activity of the intestinal mucosa greatly affect the rate of absorption.
- Lymph flow: Obstruction of the thoracic duct hinders fat absorption but does not abolish it completely due to the presence of other lymphatic collaterals.
- Proper digestion: Completely digested food is easily absorbed; improper digestion is accompanied by malabsorption.
- Intestinal movements: As mentioned before, the intestinal movements and the movements of the villi greatly enhance the rate of absorption. However, excessive peristalsis hinders absorption due to hurrying the intestinal contents as in the case of diarrhea.
- Some physical and chemical factors
- Hypertonic solutions are absorbed at a slower rate than hypotonic or isotonic solutions.
- Crystalloids are absorbed according to their concentration gradients between the intestinal lumen and plasma.
- Increased intra-intestinal pressure increases the rate of absorption.
- Solubility: solubility of the substances is necessary for their proper absorption, for example, bile salts facilitate absorption of fat and fat-soluble vitamins by dissolving them. Also, absorption of calcium is increased when the reaction of the intestinal contents is acidic because the solubility product is increased in this acidic medium.
You can download Science online application on Google Play from this link: Science Online Apps on Google Play
Small intestine constituents, Regulation, function and Digestion in the small intestine
Small intestine function, anatomy, parts, Arterial supply of the duodenum, midgut & hindgut
Histological structure of stomach, Fundic glands of Stomach & Gastric musculosa
Large Intestine function, parts, length, anatomy & Relations of the rectum