Regulation of stomach emptying, Causes of vomiting and Nervous pathway of reflex vomiting
Emptying of the gastric contents is promoted by antral peristalsis waves and prevented by resistance of the pylorus. Antral peristaltic waves provide a pumping action, which is called the “pyloric pump”. Normally the force of tonic contraction of the pyloric sphincter is weak, leading to its incomplete closure and easy passage of fluids through it.
Stomach emptying
This force is sufficient to prevent the passage of semisolid chyme into the duodenum except in the presence of strong antral peristaltic waves which drive food toward the duodenum. Pyloric sphincter and antral peristaltic waves play their role in emptying the stomach via many stimuli from the stomach and duodenum.
Regulation of stomach emptying
I) Gastric factors
- The volume of the gastric contents: Distension of the stomach increases the rate of emptying of the stomach through a nervous mechanism. The rate is directly proportional to the square root of food volume in the stomach.
- Effect of gastrin hormone on stomach emptying: As previously mentioned stretch of the stomach wall and the presence of certain types of food in the stomach release gastrin hormone, which stimulates both gastric secretion and motility. It increases the activity of the pyloric pump and relaxes the pyloric sphincter, i.e. it enhances the emptying of the stomach.
II) Duodenal factors
Feedback mechanisms from the duodenum are very important to slow down the rate of evacuation of the stomach when the small intestine is already filled. These mechanisms include:
a- Enterogastric reflex
When chyme enters the duodenum reflex inhibition of antral peristalsis associated with contraction of the pylorus occurs (enterogastric reflex) this is mediated in three ways; as a local enteric reflex, a prevertebral ganglionic and vago-vagal reflex, This is the most important factor in controlling the rate of emptying of the stomach, The most important stimuli for enterogastric reflex are the irritants and acids in the duodenal chyme, Acids are prevented from the release in the duodenum to allow time for neutralization by pancreatic and other secretions.
b- Hormonal factors
Cholecystokinin is released from the jejunal mucosa in response to fatty chyme, This hormone blocks gastric motility by competitive inhibition of the gastrin hormone, Secretin is secreted from the duodenum in response to acid chyme and it decreases gastric motility.
Gastric inhibitory peptide (GIF) is released from the upper small intestine in response to fat and to a lesser extent in response to carbohydrates, It inhibits gastric acid secretion and motility, Its main function is probably to stimulate the release of insulin from the pancreas after a meal.
Somatostatin is secreted in the enteric plexus of the GIT, It inhibits the secretion of gastrin and inhibits gastric emptying, Vasoactive intestinal peptide (VIP) mainly decreases HCI secretion and motility.
III) Some other factors which affect gastric emptying
- Chemical agents: Cholinergic drugs, sodium bicarbonate, coffee, alcohol, and vitamin B complex members are stimulants to gastric movements, Adrenergic drugs, cholinergic blockers (as atropine), smoking, and bacterial toxins depress stomach emptying.
- Emotions: In anxiety and anger, gastric motility and secretion are greatly increased, while fear, pain, depression, sadness, and muscular exercise depress them, Persistent excitation leads to peptic ulceration.
- Consistency of food: Emptying of fluids is more rapid than semisolids, which in turn are emptied faster than solids, Solid food takes a long time until it is converted to “chyme” by proper mixing and partial digestion by gastric juice.
IV) Autonomic stimulation
Sympathetic inhibits motility while parasympathetic increases motility.
V) Type of food
Proteins (particularly meat) stimulate the release of gastrin → increase gastric motility and inhibit the pyloric sphincter → faster emptying. Fat (heavy meal) inhibits motility and emptying. The entry of fats and fatty acids in the duodenum releases some duodenal hormones that delay gastric emptying. They decrease gastric motility and increase the tone of the pyloric sphincter.
Vomiting
It is the outward expulsion of the gastric contents (also intestinal contents), through the oesophagus, pharynx, and mouth, A large number of plain and voluntary muscles share in this complex act, It is preceded by a sense of nausea and profuse salivation from the buccal, pharyngeal, and esophageal mucosa.
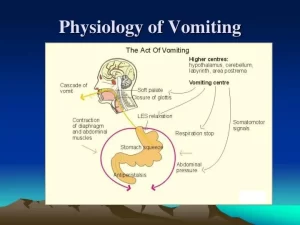
Nervous pathway of reflex vomiting
- Receptors and afferents: may arise anywhere in the body according to the cause of vomiting.
- Centre: The “vomiting center” in the medulla oblongata. It consists of various neurons that control the different components of the vomiting act.
Efferents
- 5th, 7th, 9th, 10th, and 12th cranial nerves to the upper part of the gastrointestinal tract.
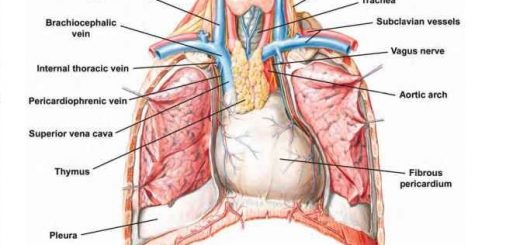
- Phrenic nerves to the diaphragm.
- Spinal nerves to the muscles of the anterior abdominal walls.
Response = Peripheral mechanism of vomiting
The act of vomiting results from a squeezing effect of the abdominal muscles associated with the sudden opening of the oesophageal sphincters. This occurs via the following steps:
- Contraction of the diaphragm, the anterior abdominal wall muscles, and the pelvic floor, leads to the rise of the intra-abdominal pressure.
- Relaxation of the body and fundus of the stomach, relaxation of the oesophageal sphincters.
- Contraction of the pyloric portion of the stomach. In this condition, the squeezing effect of the elevated intra-abdominal pressure drives the stomach contents into the relaxed oesophagus.
- The protective reflexes that prevent the passage of vomitus in the respiratory passages take place; these are elevation of the soft palate, raising of the larynx, and closure of the glottis. Holding of breath occurs until the vomitus is washed out. Sometimes antiperistalsis may occur to drive the duodenal contents into the stomach, and consequently, the vomitus contains bile.
Causes of vomiting
The causes of vomiting can be grouped into:
1) Central causes
Any factor that affects the vomiting center, either by:
- Direct stimulation of the vomiting center in the medulla oblongata as in cases of increased intracranial pressure due to brain tumors or other lesions.
- Indirect stimulation of the vomiting center by certain circulating chemical agents in the blood. These influence the vomiting center indirectly through the chemoreceptor trigger zone located in the area postrema which is unprotected by the blood-brain barrier, and this would stimulate the center.
These substances may be:
- Exogenous emetics e.g. tartar emetic, emetine, and morphine.
- Endogenous emetics: e.g. blood urea which accompanies uraemia.
2) Peripheral causes (Reflex vomiting)
Reflex stimulation of the center may occur by afferent impulses that arise from different parts of the body in addition to the irritation of the mucosa of the upper gastrointestinal tract, e.g. by mechanical stimulation of the posterior part of the tongue or drinking salty solution. Irritation of the following organs by inflammation. neoplastic growth or ulceration is associated with vomiting:
- The gastrointestinal tract: from the pharynx to the colon.
- Other abdominal organs: e.g. kidneys.
- Extra-abdominal organs: e.g. cardiac or chest conditions. Irritation of the vestibular nuclei mediates nausea and vomiting associated with vertigo e.g. motion sickness.
3) Psychogenic vomiting
Vomiting occurs in psychic troubles (without any organic diseases) or by conditioned reflexes through visual, olfactory or gustatory stimuli: e.g. “nauseating smells” and “sickening sights.”
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Constituents of the gastric juice, Gastric motility & types of movements occur in the stomach
Physiology & functions of Stomach, Composition of gastric secretion
Histological structure of stomach, Fundic glands of Stomach & Gastric musculosa
Stomach parts, function, curvatures, orifices, peritoneal connections & Venous drainage of Stomach
Abdomen muscles, Blood Supply of Anterior Abdominal Wall & Rectus Sheath content
Histological organization of pharynx, Structure & function of esophagus