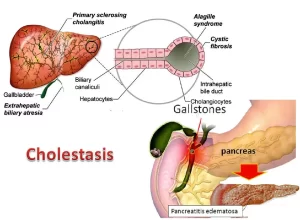
Liver Cholestasis types, causes, features, symptoms, diagnosis and treatment
Cholestasis results from interference with bile flow anywhere from the basolateral membrane of the hepatocyte to the entry of the bile duct into the duodenum. Cholestasis can occur both with and without jaundice. Composition of bile: water (85%), bile acid, phospholipids, proteins, bilirubin, and cholesterol.
Types & Causes of Cholestasis
A. Extrahepatic cholestasis.
Anatomy of Extrahepatic cholestasis: obstruction occurs from the hilum of the liver down to the duodenum, The bile flow is interrupted in its passage from the porta hepatis to the duodenum because of intraluminal obstruction, obliterating disease of the biliary duct or compressions of the extrahepatic bile ducts.
Causes
- Obstruction in the area of the papilla of Vater: Inflammation, Choledocholithiasis, and Neoplasia.
- Obstruction in the area of bile ducts: Choledocholithiasis, Cholangiocarcinoma, Postoperative stricture (following cholecystectomy, the common bile duct may be ligated), Pancreatic cyst, Pancreatitis, Pancreatic head carcinoma, Gall bladder carcinoma, and Fascioliasis.
B. Intrahepatic Cholestasis
Anatomy of intrahepatic cholestasis: there’s obstruction from the basolateral membrane down to the hilum of the liver, It is due to temporary or permanent obstruction of the intrahepatic bile ducts.
Causes
- Acquired causes: Alcohol/autoimmune hepatitis / chronic hepatitis/cirrhosis/ hyperthyroidism/
- Endotoxins: (any patient with severe infections, there will be endotoxemia and probably will develop cholestasis).
- Focal changes in the liver: means that the normal soft parenchyma of the liver gets changes like Adenoma/hemangioma /cyst/ tumors /abscesses /Hodgkin disease /parasites /hepatolithiasis /Caroli syndrome (in which there are cystic dilatations of the hepatic duct).
- Disseminated changes of the liver: Sarcoidosis/ tuberculosis/mucoviscidosis.
- Infiltrative changes of the liver: In which the soft liver is infiltrated by excessive cells leading to compression of the bile ducts E.g., Leukemia/ amyloidosis/ primary storage disease.
- The inflammatory proliferation of the bile ducts: Primary biliary cirrhosis, Primary sclerosing cholangitis.
- Recurrent intrahepatic cholestasis of pregnancy: The disease is due to recessive autosomal transmission where there is a defect in phosphatidylcholine transport and a concurrent sensitivity to estrogen or inhibition of bile acid transport due to an increase in estrogen /progesterone metabolite. The syndrome is characterized by severe itching in hands and soles during the 2nd & 3rd trimesters, this is followed by jaundice, It is managed by: cholestyramine/UDCA and medium-chain fatty acid.
- Drugs: ACE inhibitors/ atenolol/ azathioprine/b-blockers/ haloperidol/ ketoconazole/ penicillamine.
- Benign recurrent Intrahepatic cholestasis: Recessive autosomal transmission, It can occur at any age but not before 9 months, It may be triggered by infections, toxins, or allergens.
- Progressive familial Intrahepatic cholestasis: Every component of bile is excreted through a pump (several channels for excretion of the bile constituents.
The canalicular membranes contain several ATP-dependent export pumps:
- The multidrug resistance-1 P-glycoprotein (MDR1) transports organic cations into bile.
- Phospholipid transporter multidrug resistance-3 P-glycoprotein (MDR3).
- Canalicular multi-specific organic anion transporter (CMOAT), which is also termed the multidrug resistance-associated protein 2 (MRP2).
- Canalicular bile salt export pump (BSEP), which is also known as the “sister of P-glycoprotein” (SPGP).
- Chloride-bicarbonate exchange, glutathione (GSH) transport, and the product of the FIC1 (familial intrahepatic cholestasis type 1) gene, which has been redesignated ATP8B1, a P-type ATPase that probably transports amino phospholipids.
PFIC can now be subdivided into:
PFIC-1
It was previously recognized as Byler’s disease and is due to a mutation in an aminophospholipid transporter. The gene mutation occurs in other epithelial body tissue which explains the multisystem manifestation of the disorder. The disease manifests around the first year of life and is characterized by pruritus and hepatomegaly as well as elevated bile acids in the serum. Progressive cholestasis leads to, malabsorption, and developmental disorder. Byler’s disease is fatal after 3-20 years.
Byler’s syndrome: mutations in genes PFIC 2-4
The treatment of this disorder is antipruritic agents and UDCA (Ursodeoxycholic acid).
PFIC-2
A defect in the bile salt export pump BSEP also known as the “sister of P.glycoprotein,” SPGP) which causes jaundice in infancy associated with nonspecific giant cell hepatitis.
PFIC-3
Mutations of the MDR3 gene abolish phospholipid secretion into bile and this leads to liver damage with extensive bile ductular proliferation, pruritus, and cirrhosis in childhood, The same defect may be related to intrahepatic cholestasis of pregnancy.
PFIC-4
There is genetically deficient 3β-hydroxy C-27 steroid dehydrogenase resulting in impaired bile acid metabolism. There is no pruritus; bile acids and gamma Gt (glutamyl transferase) are reduced, but conjugated bilirubin increases.
Zellweger Syndrome
It is the autosomal recessive genetic absence of peroxisomes in the liver and kidneys caused by mRNA mutation of peroxisome. This impairs bile acid synthesis and compromises the β-oxidation of fatty acids, Clinically, there are skeletal and nervous system abnormalities and polycystic kidney, Laboratory findings; hypoprothrombinemia, cholestasis, jaundice, and hypersiderinemia. The prognosis is poor and the patient dies after a few months.
Clinical features of cholestasis
Jaundice develops slowly.
Pruritus (the hallmark of cholestasis)
It is often attributed to retained bile acids that irritate the nerve endings, Cholestyramine binds many compounds and thus its success in treating the pruritus of cholestasis does not incriminate one agent. Recently, it has been suggested that opiates have a role in itching cholestasis. The opiate antagonist naloxone decreases scratching.
Xanthomas
The planous varieties (xanthelasma) are flat or slightly raised, yellow, and soft. They may also be seen in the palmer creases, below the breast and on the neck, chest, or back. The tuberous lesions appear later and are found on extensor surfaces, especially the wrists, elbows, knees, ankles, and buttocks on pressure points, and in scars.
Retention of cholesterol and hypercholesterolemia, which will be deposited around the eyes (as xanthelasma) and as tuberous elevations in the hands (aş xanthoma). The liver is usually enlarged with a firm, smooth, non-tender edge. Splenomegaly is unusual except in biliary cirrhosis where/PHTN has developed or if infection is present.
Feces
In complete biliary obstruction, there’ll be no urobilinogen reaching the stool and there’ll be no urobilin or stercobilin so the stool will be light in color. Fecal color gives a good indication of whether cholestasis is total intermittent or decreasing.
Steatorrhea (bulky, fatty, offensive stool that floats on the surface of water due to increased fat content); Bile salts, deficient in the intestine in cholestasis, are essential for the absorption of dietary fat. It is proportional to the depth of jaundice. Stools are loose, pale, bulky, and offensive.
Hepatic osteodystrophy
In prolonged cholestasis due to impaired absorption of vit D and calcium, Bone pain is frequent. (osteopenia), Bone biopsy may reveal either osteomalacia or, more often, osteoporosis (fractures if it’s prolonged).
Changes in copper metabolism
Approximately 80% of absorbed copper is normally excreted in the bile and lost in the feces, Copper will accumulate and pigment’ corneal rings resembling Wilson’s disease in which there are Kayser-Fleischer rings which are seen rarely.
Fat-soluble vitamins and coagulation factors (Impaired absorption of fat-soluble vitamin Vitamin height blindness.
Vitamin A: night blindness. Vitamin K: Prothrombin time is prolonged. This is restored to normal by intra-muscular vitamin K1 therapy. (hypoprothrombinemia), Vitamin E: Cerebellar ataxia, posterior column dysfunction, peripheral neuropathy, and retinal degeneration.
Extra-hepatic effects
- Cardiovascular responses are abnormal and peripheral vasoconstriction in response to hypotension is impaired. Which the patient may develop bradycardia and postural hypotension.
- The kidneys have an increased susceptibility to hypotension and hypoxic damage.
- The processes involved in responding to sepsis and in wound healing are impaired.
- The prolonged prothrombin time is correctable with vitamin K but coagulation may still be abnormal) through platelet dysfunction.
- The gastric mucosa is more susceptible to ulceration.
Biochemistry
The principle biochemical symptom of cholestasis is the rise in serum bile acids, Serum alkaline phosphatase is raised, usually to more than three times the upper limit of normal. Serum γ-glutamyl transpeptidase is raised. The rises are due to increased synthesis or release of enzymes from liver membranes. Total serum cholesterol increases but not constantly.
Urine
Conjugated bilirubin is present. Urinary urobilinogen is excreted in proportion to the amount of bile reaching the duodenum.
You can subscribe to science online on Youtube from this link: Science Online
You can download Science Online application on Google Play from this link: Science Online Apps on Google Play
Conjugated hyperbilirubinemia cause, symptoms and treatment
Unconjugated hyperbilirubinemia causes, symptoms, diagnosis and treatment
Jaundice symptoms, types, cause, treatment and What is the source of bilirubin?
Hepatocellular carcinoma symptoms, stages, risk factors, diagnosis, and treatment
Liver failure, symptoms, stages, cause, treatment, Acute on chronic liver failure (ACLF)
Ascites cause, grades, symptoms, diagnosis and Treatment of cirrhotic ascites
Hepatic Artery Embolization, Importance & risks of Embolization therapy for Liver cancer
Interventional radiology types, Robotic endovascular systems advantages & disadvantages