Factors regulating food intake, Causes and Effects of complete starvation
Hunger is a craving for food and is associated with objective sensations such as hunger contractions of the stomach. Appetite is a desire for specific types of food instead of food in general satiety means a feeling of fulfillment in the quest for food (the opposite of hunger).
Neural centers that regulate food intake
I) Hypothalamic centers
- The feeding (hunger) center lies in the lateral hypothalamus. When it is stimulated in experimental animals, it causes ‘hyperphagia” (eating behavior). On the other hand, the destruction of this center causes a lack of the desire for food, progressive weight loss. muscle weakness and fatal anorexia. The feeding center is chronically active and directly excites the emotional drive to search for food. It is transiently inhibited by the satiety center after food ingestion.
- The satiety center. It lies in the ventromedial nuclei of the hypothalamus. Its stimulation causes aphagia (complete satiety and cessation of eating) whereas its destruction causes hyperphagia and extreme obesity (hypothalamic obesity syndrome).
II. Other centers
- The amygdala and the prefrontal cortex: They are closely coupled with the hypothalamus. Their destruction causes omniphagia; a type of moderate hyperphagia leading to attempting to eat all sorts of objects (regardless of type and quality).
- Brain stem centers: They control the actual mechanisms of feeding as salivation. chewing and swallowing. They are excited by signals from the hypothalamus.
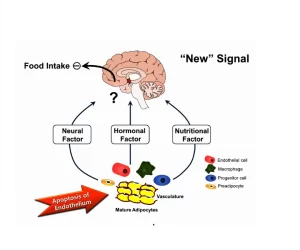
Factors regulating food intake
Long term regulation
a) Nutritional regulation: When the nutrient stores fall below normal, the feeding center becomes highly active and the person exhibits increased hunger. On the other hand, when the nutrient stores are abundant, the person loses hunger and develops a state of satiety. Several theories explain nutritional regulation:
- The glucostatic theory: The activity of the satiety center is affected by the level of glucose utilization of cells within the center called “glucostats”. When the blood glucose level decreases, their glucose utilization is low, their activity is decreased and the activity of the feeding center becomes unchecked and the individual is hungry. On the other hand, when the glucose utilization of the glucostats is high, their activity is increased and the feeding center becomes inhibited.
- The lipostatic and aminostatic theories: The same neurons which are affected by blood glucose level are also affected by blood concentration of breakdown products of lipids and by amino acids.
b) Effect of environmental temperature (thermostatic theory): Exposure to cold causes a tendency to over eating because it increases the metabolic rate and provides increased fat for insulation while exposure to heat results in under eating.
c) Feedback signals from adipose tissue eating. The hypothalamus senses energy storage through the action of a hormone called leptin, released from adipocytes. When the amount of adipose tissue increases ( = excess energy storage), adipocytes produce an increased amount of leptin that circulates in the blood. It crosses the blood brain barrier, binds with leptin receptors at multiple sites in the hypothalamus and initiates the following actions to decrease food intake and increase energy consumption:
- Decreased production of appetite stimulators in the hypothalamus as neuropeptide Y.
- Increased production of substances that decrease food intake in the hypothalamus as a corticotropin-releasing hormone.
- Increased sympathetic nerve activity which increases the metabolic rate and energy expenditure.
- Decreased insulin secretion which decreases energy storage.
Short term regulation
It prevents over eating, because nutritional feedback mechanisms take at least an hour before enough quantities of food substances are absorbed into the blood and cause inhibition of eating.
a) Alimentary factors
- Gastrointestinal filling: distention of the gastrointestinal tract, especially the stomach and the duodenum, sends inhibitory signals via the vagi to the feeding center.
- Hormones: the presence of food in the stomach and the duodenum causes the release of hormones that suppress the feeding center e.g. cholecystokinin, glucagon, insulin, and calcitonin.
- Oral factors: chewing, tasting, salivation and swallowing cause weak inhibition of the feeding center, that lasts for 20-40 minutes.
b) Psychological factors: Cultural, environmental factors and past experiences relative to the sight, smell and taste of food affect food intake.
Physiology of starvation
Starvation is the absence of food intake, except for water. It may be partial or complete.
Causes of starvation
- Decreased availability of food as in famines and poverty.
- Refusal of food intake either due to psychological causes such as anorexia nervosa or voluntary starvation.
- Gastrointestinal causes as malabsorption syndrome and cancer esophagus.
Effects of complete starvation
1- Depletion of food stores in the body tissues: An average 70 Kg man has about 0.1 Kg glycogen in his liver, about 0.4 Kg of glycogen in his muscles, and 12 Kg of fat. During starvation, the subject passes through the following phases:
- During the first day of starvation, the body tissues use carbohydrates for energy. These carbohydrates are derived from glycogen stores in the liver and muscles. They are totally consumed within the first day.
- After glycogen stores are totally depleted, fat and easily mobilizable proteins are converted by gluconeogenesis into glucose to keep its level at the fasting level.
- After that fat becomes the only source of energy. Ketone bodies can be utilized by the brain cells to provide about 2/3 of their energy needs.
- At the end, tissue proteins are rapidly catabolized. When they have been depleted to about one-half their normal level, death occurs.
2- Vitamin deficiency: After a week, mild vitamin deficiencies usually begin especially the water-soluble vitamins (vit B and C). After several weeks, severe deficiencies can occur which add to the debility leading to death.
3- Gradual weight loss: The individual loses about 1 Kg/day for the first 10 days, then, 0.3 Kg /day afterwards. Body organs also decrease in size; the liver, the kidneys, the heart, and the gastrointestinal tract, except for the brain, which is spared.
4- The decreased activity of both endocrine and exocrine glands
5- Decreased basal metabolic rate and body temperature.
6- Depressed cardiovascular functions: bradycardia, decreased cardiac output, lowered arterial blood pressure, and postural hypotension.
7- Depressed mental functions and increased sleeping hours. Psychological disturbances appear in the form of personality changes and the person becomes self-centered.
8- Hunger pains occur but disappear after 2-3 days. Atrophy of the intestine and decreased digestive secretions lead to diarrhea.
9- Blood changes: Blood glucose concentration is kept at the fasting level by gluconeogenesis. Anemia, hypoproteinemia (causes edema), ketosis, starvation lipaemia (due to fat mobilization) and decreased alkali reserve (used to buffer the ketoacids).
10- Urinary changes as Ketonuria.
11- Edema mainly due to due to hypoproteinemia
12- Death usually occurs about 60 days from the start of starvation. The terminal event is intractable diarrhea.
You can download Science online application on Google Play from this link: Science online Apps on Google Play
Uses of oxygen debt, Factors affecting Metabolic rate, and SDA of food
Metabolism, Energy balance, Basal metabolic rate and Factors affecting respiratory exchange ratio
Functions of Kidneys, Role of Kidney in glucose homeostasis, Lipid and protein metabolism
Factors affecting cardiac output, Stroke volume, Heart rate and blood pressure